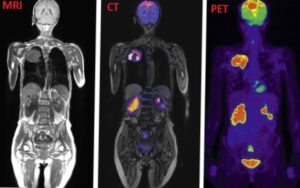
Accurate imaging is the cornerstone of modern radiation oncology. Before delivering any radiation dose, oncologists must know exactly where the tumor is, what structures it’s invading, how biologically active it is, and what organs are at risk nearby. Computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) each provide unique insights into anatomy and physiology that are critical to every step of radiotherapy, from treatment planning and target delineation to monitoring response and adapting therapy.
This article explores how each imaging modality works, their specific roles in radiotherapy, and how they work together to deliver safer, more effective cancer treatment.
Article Summary
What is a CT scan?
The CT scan machine consists of an X-ray emitting tube and detectors that capture multiple images from different angles around the patient. The X-ray beams pass through tissues with varying densities: bone, muscle, fat, and air, which absorb radiation differently. This information allows the computer to create a detailed 3D model of the patient’s anatomy. Sometimes, a contrast agent (such as iodine or barium) is used to make certain organs, blood vessels, or tissues more visible on the scan.
Risk considerations
While CT provides excellent anatomical detail, it’s important to be aware of safety considerations. During CT scans patients are exposed to higher doses of ionizing radiation compared to standard X-rays, which can slightly increase the lifetime risk of cancer, especially with repeated scans. To minimize this risk, the ALARA principle (As Low As Reasonably Achievable) is applied, meaning imaging protocols aim to use the lowest radiation dose possible while still obtaining quality diagnostic images.
Clinical Use in Radiotherapy
CT imaging plays a crucial role in radiotherapy planning. It provides detailed 3D anatomical information, allowing accurate localization of tumors and surrounding healthy tissues. This enables precise dose calculation and beam arrangement to maximize tumor control while minimizing exposure to normal organs.
- Simulation and planning: CT is the standard imaging method for radiotherapy planning, providing 3D anatomical data and information about positioning.
- Dose calculation: CT data provides electron density information, essential for dose modeling in treatment planning systems.
- Target volume delineation: Though it offers less soft tissue contrast than MRI, CT is sufficient for many tumor locations, such as lung or bone.
- Motion management: 4D-CT scans capture tumor motion (e.g., due to breathing) to ensure accurate dose delivery in thoracic and abdominal cancers.
- Image-guided radiotherapy: The Cone-Beam CT (CBCT) integrated into linear accelerators allows real-time verification of the patient’s positioning.
- Brachytherapy planning: Common in gynecological, prostate and head & neck cancers the CT helps localize applicators and nearby structures in internal radiation therapy.
- Follow-up and surveillance: Post-treatment CT is used for monitoring tumor response, detecting recurrence or complications and for evaluating radiation-induced changes in normal tissues.
What is an MRI scan?
The MRI (Magnetic Resonance Imaging) is another type of medical imaging device which uses magnetic fields and radio waves instead of X-rays. The radio waves interact with the hydrogen nuclei (protons) inside the body emitting signals that are detected and reconstructed into images. There are two key sequences – T1 and T2 – which are different for various tissue types (fat, water, muscle, tumor), producing the strong soft tissue contrast characteristic to this type of imaging.
Risk considerations
MRI is considered a safe imaging modality, primarily because it does not involve ionizing radiation. However, careful assessment is essential for patients with certain implants, such as pacemakers, cochlear implants, or prosthetic devices, as these may be incompatible with MRI technology. The procedure itself can be quite loud, and depending on the area being examined, it may last up to two hours.
Clinical Use in Radiotherapy
- Tumor delineation: Because of the superior soft tissue contrast, the MRI is ideal for accurately outlining tumors particularly in brain, prostate, head and neck, pelvis and spine cancers.
- Biological targeting: MRI sequences can assess tumor cellularity, perfusion and hypoxia, which can guide dose escalation to more aggressive tumor regions.
- MRI-guided radiotherapy: With the recent development of MR-Linacs, real-time MRI guidance during treatment is possible.
- Monitoring treatment response: Useful for differentiating between residual tumor, inflammation and necrosis.
- Post-treatment surveillance and recurrence detection: MRI is often used in follow-ups, especially in areas like the brain.
What is a PET scan?
Positron Emission Tomography (PET) is a type of nuclear medicine scan that shows how tissues and organs are working by highlighting areas of metabolic activity. Before the scan, the patient is given a small amount of a radioactive substance, usually a form of sugar called FDG, which is labeled with a tiny radioactive tracer. Active cells, like cancer cells, absorb more of this sugar, and the tracer helps to show where these cells are in the body. Other non-specific active cells like inflammatory cells or healing areas might also light up on a PET scan, which is why it is important to interpret the scan in a clinical context.
Some common cancers where PET is an important imaging tool are lung, head and neck, esophageal, cervical, rectal cancers and lymphomas.
Clinical Use in Radiotherapy
- Tumor detection and staging: (usually PET/CT) helps identify primary tumors, nodal involvement, and distant metastases. It improves staging accuracy, which is essential for deciding whether radiotherapy is appropriate.
- Target volume delineation: PET identifies metabolically active tumor regions, helping define the tumor volume more precisely, while sparing the surrounding healthy tissue.
- Treatment planning optimization: PET can distinguish viable tumors from necrosis, inflammation, or post-treatment changes, allowing better customization of dose distribution.
- Response assessment: PET is used after or during radiotherapy to assess tumor response (e.g., reduction in metabolic activity).
- Recurrence detection: PET provides high sensitivity for detecting tumor recurrence vs. post-treatment scarring or fibrosis, which can look similar on CT or MRI.
Comparison: CT vs. MRI vs. PET
In radiation oncology, imaging plays a critical role in diagnosis, staging, treatment planning, and response assessment. Each imaging modality, CT, MRI, and PET, offers unique strengths that contribute to accurate tumor localization, target volume delineation, and monitoring.
|
FEATURE |
CT |
MRI |
PET |
|
Basic technology |
Uses X-rays and computer processing to create cross-sectional images |
Uses strong magnetic fields and radio waves |
Uses radioactive tracers to visualize metabolic activity |
|
What it shows |
Bone, tumors, lung/chest pathology, anatomical detail |
Soft tissue structures, tumor extent in brain/spine/pelvis |
Tumor metabolism, viability, and functional changes |
|
Radiation |
Yes (ionizing radiation) |
No radiation |
Yes (radioactive tracers) |
|
Scan time |
Quick (typically 5–10 minutes) |
Longer (20–60 minutes) |
Longest (30–90 minutes) |
|
Cost |
Moderate |
Expensive |
Most expensive |
|
Noise level |
Moderate |
Very loud (requires ear protection) |
Quiet to moderate |
|
Enclosed space |
Partially enclosed |
Fully enclosed (tube-like) |
Fully enclosed |
|
Contraindications |
Pregnancy, contrast allergies |
Metal implants, pacemakers, claustrophobia |
Pregnancy, recent surgeries, blood sugar disorders |
|
Best for |
Quick localization, bone & chest tumor staging, treatment planning |
Delineation of soft tissue tumors (CNS, prostate, head & neck cancers) |
Identifying active tumor tissue, detecting metastases |
While each imaging modality holds its strengths and limitations, in clinical practice, combining modalities provides a comprehensive view of the tumor and surrounding anatomy in radiotherapy. CT forms the foundation for treatment planning and dose calculation, MRI enhances soft tissue contrast for more accurate tumor delineation, and PET offers metabolic insights to identify active disease. When fused in planning systems, these modalities work synergistically to improve targeting precision, minimize radiation to healthy tissue, and support more personalized, effective treatment strategies.
Common patient concerns
For many patients, undergoing imaging as part of cancer treatment can bring up concerns about safety, comfort, and side effects. CT, MRI, and PET scans each play a vital role in radiotherapy, but they also come with different experiences and precautions. Understanding what to expect can help ease anxiety and prepare patients for a smoother process.
1. General safety considerations
- CT scans use X-rays, which involve ionizing radiation. While the dose is low and carefully controlled, it’s important to avoid unnecessary exposure, especially during pregnancy.
- MRI scans do not use radiation but rely on powerful magnets. Patients with metal implants (like pacemakers or aneurysm clips) must be screened beforehand to ensure safety.
- PET scans involve a small amount of radioactive tracer. The radiation dose is low, but precautions are needed, especially around pregnant women and young children after the scan.
2. Claustrophobia and anxiety
Lying still inside a scanning machine can be stressful for some patients, particularly in MRI and PET scans, which often take longer than CT. If you’re prone to claustrophobia you should inform the medical team in advance, as many options such as mild sedatives or open MRI may be available. Most modern scanners support two-way communication, and you’ll be monitored throughout the procedure. Some breathing and relaxation exercises can also help manage anxiety.
3. Contrast Agents and tracers
To enhance image quality, some scans require substances injected into the bloodstream.
- CT and MRI may use contrast agents, typically iodine-based for CT or gadolinium-based for MRI
- PET scans use a radioactive tracer to highlight active tissue
While generally safe, these substances can cause a warm sensation, metallic taste or mild nausea and rarely, allergic reactions or issues for patients with kidney problems. Always inform your doctor about any allergies, kidney conditions or previous reactions.
4. Pregnancy and pediatric cases
- Pregnant patients should always inform their care team. MRI may be preferred over CT or PET, depending on the clinical situation.
- For children, imaging protocols are adjusted to limit radiation and ensure comfort. In some cases, sedation may be used to help young patients stay still during the scan.
5. Helpful questions to ask your doctor
- Why is this scan important for my treatment?
- Will I need contrast or a tracer? Are there risks?
- How do I prepare for the scan (e.g., fasting or medication adjustments)?
- How long will it take, and what will I experience?
- Are there alternatives if I’m anxious or have implants?
Future of medical imaging
CT, MRI, and PET scans are indispensable tools in radiation oncology, each offering unique and complementary insights. CT provides structural clarity for planning and dose calculations; MRI adds precision in soft tissue definition; and PET reveals tumor biology and metabolic activity. When integrated, these modalities enable clinicians to deliver more targeted, adaptive, and effective cancer treatments.
As imaging technology continues to advance, its role in shaping the future of personalized radiotherapy will become even more critical. Advances in artificial intelligence (AI) are enabling faster image analysis, automated tumor segmentation such as the newest solution from Synaptiq – the Active Intelligence Tool, and improved decision-making for radiation planning. Hybrid imaging techniques, such as PET/MRI, are combining anatomical and functional information in a single scan, reducing the need for multiple appointments and improving accuracy. In addition, real-time imaging and adaptive radiotherapy are emerging tools that allow treatment to adjust dynamically based on changes in tumor size or patient anatomy. These innovations are paving the way toward more targeted treatments, reduced side effects, and better outcomes for cancer patients.
References:
- Hoskin PJ, Goh V. Imaging for Clinical Oncology: Radiotherapy in Practice. 2nd ed. Oxford University Press; 2021.
- Dawson LA, Jaffray DA. “Advances in Image-Guided Radiation Therapy.” J Clin Oncol. 2007;25(8):938–946. doi:10.1200/JCO.2006.09.9460
- Paulson ES, Erickson B, Schultz C, Allen Li X. “Comprehensive MRI Simulation for Radiation Therapy: MRI Simulation, MRI Alone, and Multimodality Fusion.” Med Phys. 2015;42(7):3479–3492.
- Shankar A, Jeyachandran D, Reddy S et al. “Role of FDG PET and PET/CT in the Radiotherapy Planning.” J Med Imaging Radiat Oncol. 2014;58(3):261–276.
- Hall WA, Paulson ES, van der Heide UA, et al. “The Transformation of Radiation Oncology Using Real-Time Magnetic Resonance Guidance: A Review.” Eur J Cancer. 2019;122:42–52.
- Nestle U, Kremp S, Schaefer-Schuler A, et al. “Comparison of Different Methods for Delineation of 18F-FDG PET–Positive Tissue for Target Volume Definition in Radiotherapy of Patients with Non–Small Cell Lung Cancer.” J Nucl Med. 2005;46(8):1342–1348.





